Vaccination
As of August 2020, in Scotland, no cases of invasive cervical cancer in women immunized at 12 or 13 years of age have been reported since the vaccination program began in 2008, irrespective of the number of doses.
Highly effective prophylactic vaccines are available for two of the most important cancer-causing infections, hepatitis B virus (HBV) and human papillomavirus (HPV) (see Infection).
In 2022, there were an estimated 254 million people globally with chronic HBV infection; HBV infection causes nearly one million deaths annually, mostly from cirrhosis and hepatocellular carcinoma. Vaccines to protect against hepatitis B have been available since 1982. The World Health Organization recommends that all newborns receive a hepatitis B vaccine birth dose (HepB-BD) within 24 hours of birth, followed by 2-3 additional doses, to confer full protection against hepatitis B. By 2023, 190 (98%) countries had introduced universal infant hepatitis B vaccine in the immunization schedule with 83% of children globally receiving 3-doses. However, the coverage of birth dose vaccination is still low, at 45%, with only 115 (59%) countries introducing universal HepB-BD. An additional 24 countries provide selective or restrictive HepB-BD to infants born to mothers who have chronic HBV infection (Map 35.1). Lack of country prioritization for HepB-BD introduction, and implementation challenges resulting from high rates of home births, have limited the introduction and uptake of HepB-BD in several countries.
25 years following introduction of newborn and infant hepatitis B vaccinations, incidence of primary liver cancer decreased by up to 75% in China, Taiwan and Thailand and by 100% in Alaska.
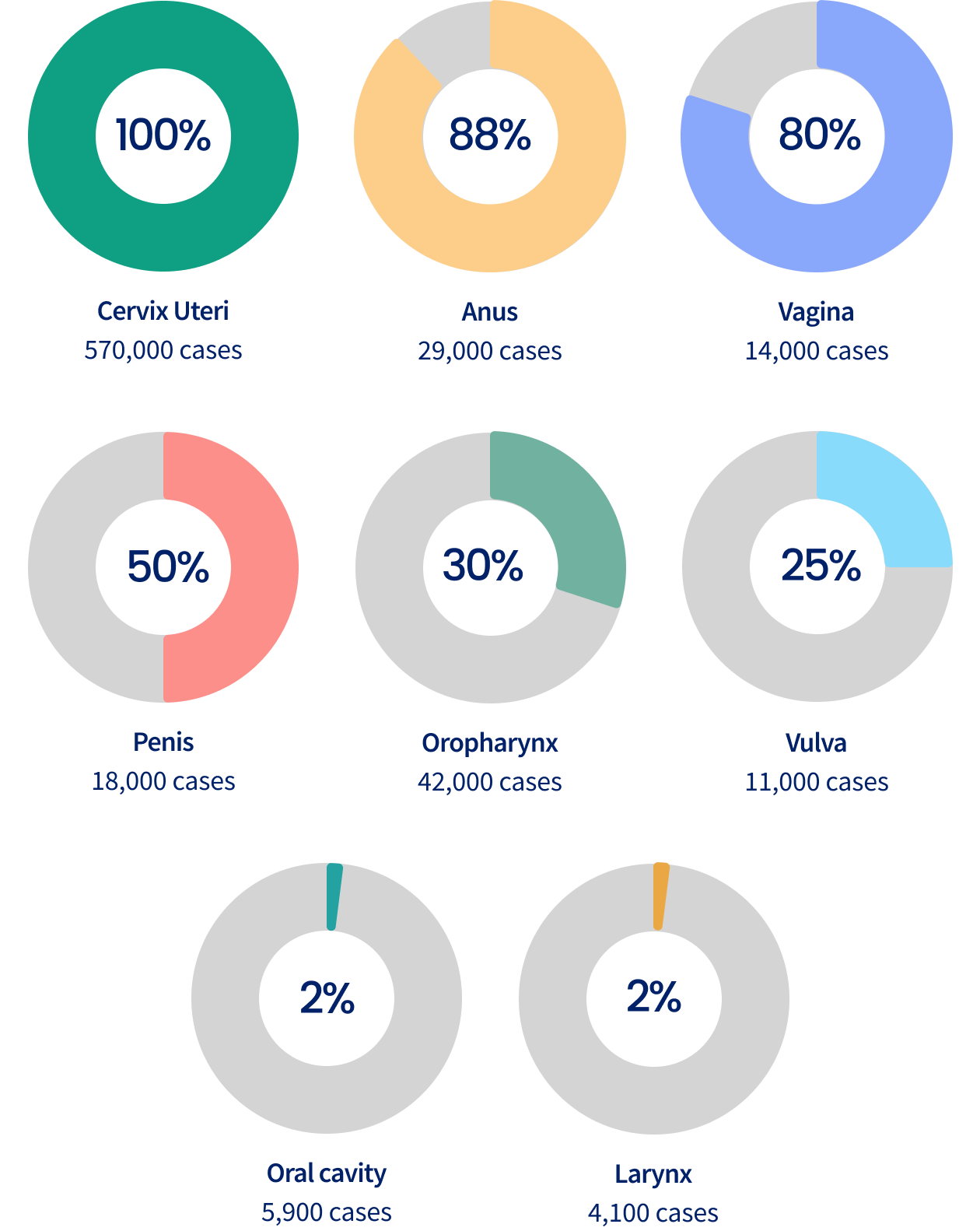
Globally, HPV is the cause of 730,000 cancers annually, including cervical, anogenital, and oropharyngeal cancers (Figure 35.1).
Cervical cancer accounts for about 80% of HPV-related cancers occurring each year worldwide.
Estimated number and proportion (%) of cancer cases attributable to Human Papillomavirus (HPV) infection worldwide by cancer type, 2020
“I stand by the HPV vaccine as a critical advancement in preventive healthcare. Its widespread adoption is essential to protect future generations from the devastating effects of HPV-related cancers.”
HPV vaccines have been available since 2006 and were first approved as a 3-dose or a 2-dose series; more recent data show that one dose is highly effective. All available vaccines protect against HPV 16 and 18, types that cause over 70% of cervical cancers and the majority of other cancers caused by HPV. The nonavalent HPV vaccine (Gardasil 9) protects against 5 additional cancer-causing HPV types and prevents over 90% of cervical cancer. In most countries, the primary target group for HPV vaccination is girls aged 9-14 years. Increasingly, countries also recommend vaccination for boys. By 2024, over 145 of 194 countries had introduced HPV vaccination programs; however, coverage has varied by region (Figure 35.2).
Globally, as of 2019, only 1 in 5 eligible girls had received HPV vaccination, far below the WHO target of 90% coverage.
Human Papillomavirus (HPV) vaccine coverage by geographic region, 2019
Girls at aged 9-14 years, first dose
Vaccine hesitancy, supply-demand imbalances, and other implementation challenges have limited HBV and HPV vaccine introductions and uptake in many countries. The Global Alliance for Vaccines and Immunization (Gavi) has provided critical financial support for HPV and hepatitis B immunization programs in low- and middle-income countries.