Early Detection
Detection of certain cancers at an early stage, along with timely treatment, permits less aggressive interventions, resulting in improved quality of life and survival.
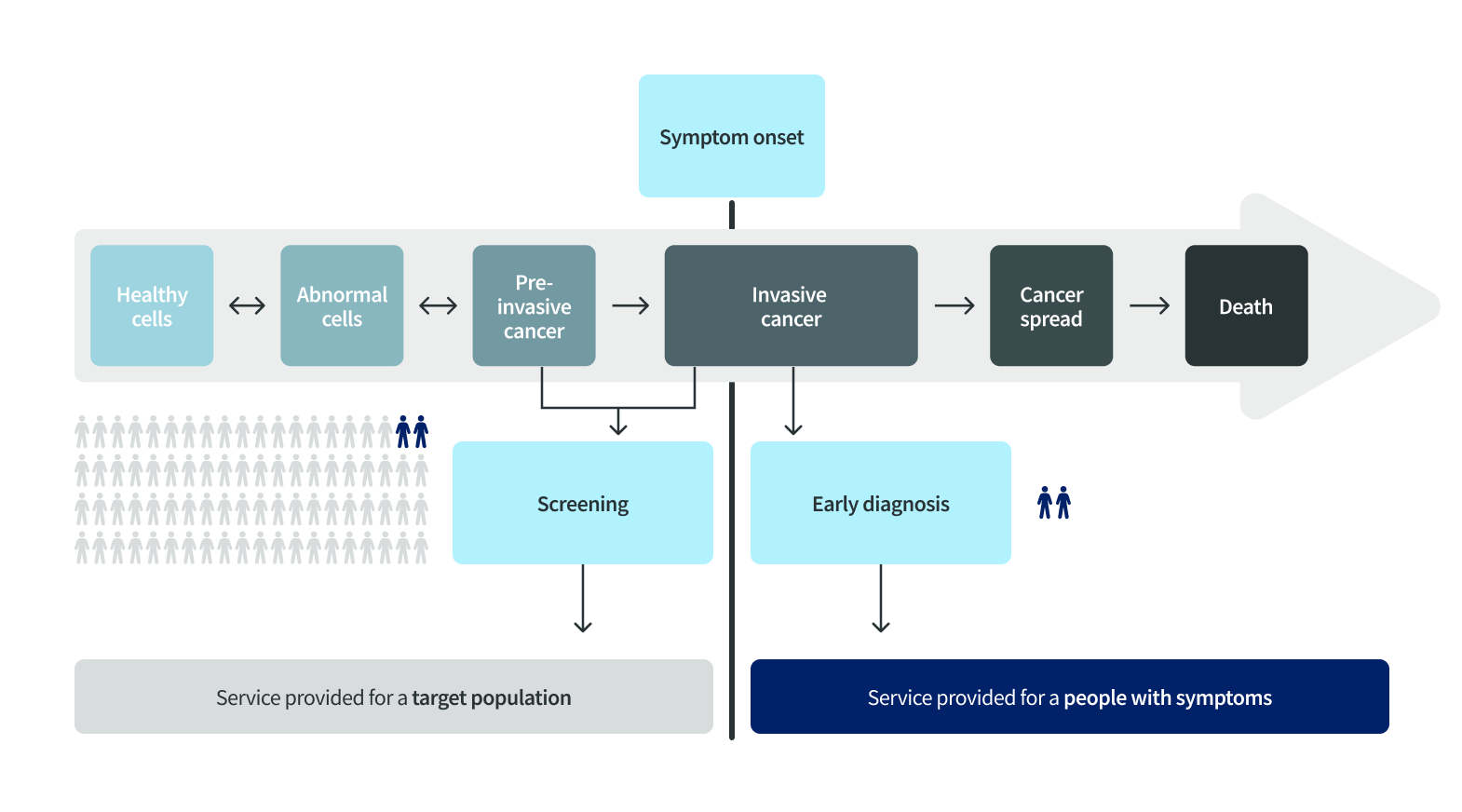
There are two approaches to early detection – screening and early diagnosis. Screening aims to detect cancers or pre-cancerous lesions in otherwise healthy and asymptomatic individuals, whereas early diagnosis identifies symptomatic cancers at the earliest possible stage (Figure 36.1).
Screening versus early diagnosis according to symptom onset
Effective screening methods for early detection of cancer are available for cervical, colorectal, female breast, and lung cancers (Figure 36.2).
Common recommendations for screening of cancers of the cervix, breast, colorectum, and lung
Footnote
The recommendations follow the WHO guidelines, except for lung cancer, which is based on the recommendations from the U.S. Preventive Services Task Force, the American Cancer Society, and the EU Mission on Cancer. *Frequencies are based on recommendations from the U.S. Preventive Services Task Force and the American Cancer Society.
Globally, only about 30% of women aged 30-49 had ever been screened for cervical cancer, ranging from 4% in Ethiopia to nearly 100% in Sweden, far below the WHO’s 70% target by 2030.
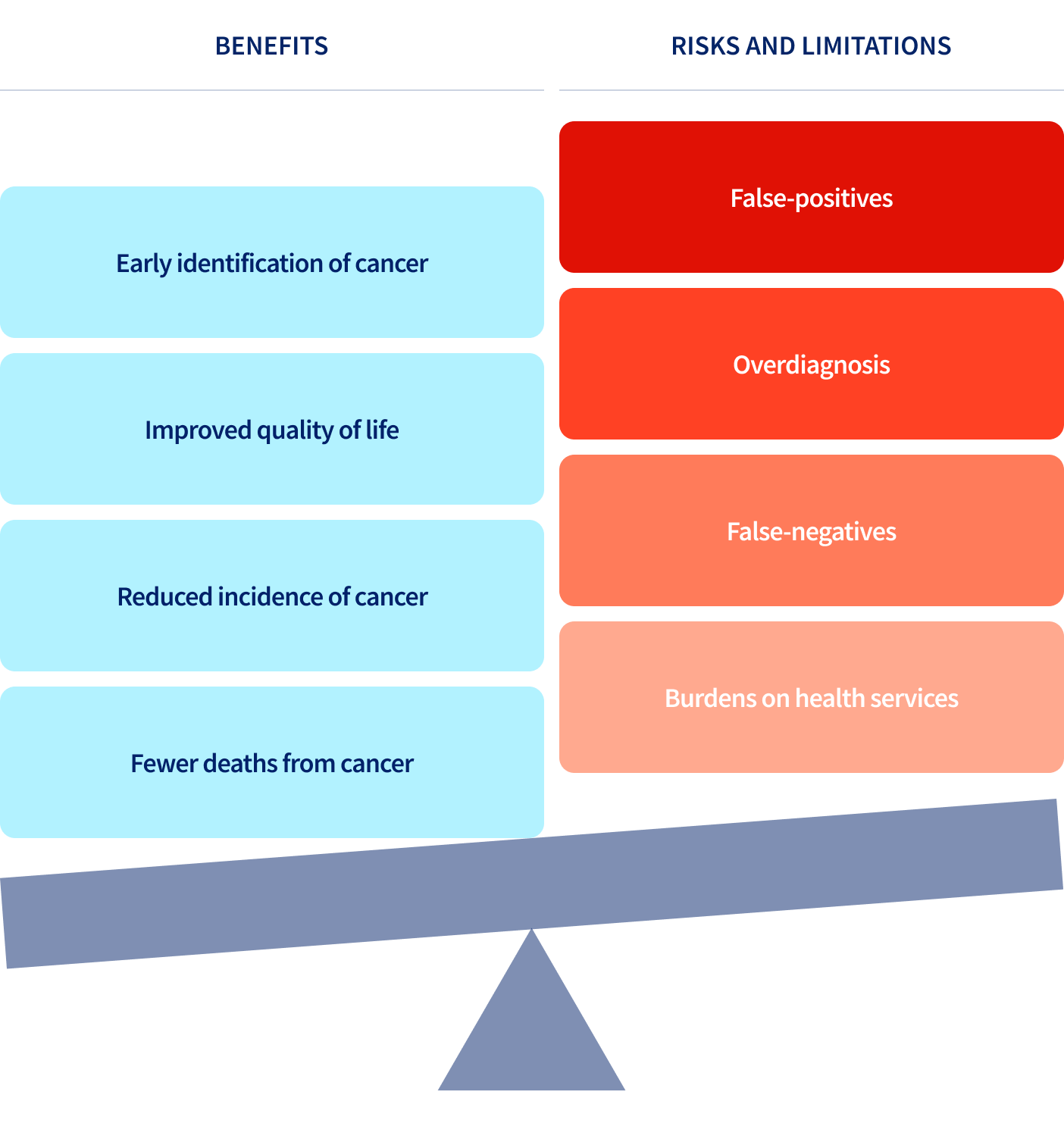
In addition, screening can prevent colorectal and cervical cancers through detection and removal of pre-cancerous lesions. However, implementing screening programs is complex and expensive. Decisions to introduce them involve balancing benefits against risks and limitations (Figure 36.3). A false positive test result can lead to significant physical, psychological, and financial harm.
Benefits, risks, and limitations of cancer screening
Many countries struggle with fiscal and infrastructural resources required to implement high-quality screening programs. This creates an uneven playing field where some populations benefit more than others. For example, there is a strong recommendation from the World Health Organization to start cervical cancer screening using human papillomavirus (HPV) detection tests at age 30 years for average risk women and at age 25 years for women living with human immunodeficiency virus. Yet, only 19 countries have rolled out HPV detection-based screening, all of which are high-income countries (Map 36.1).
“People just don’t know that you can have colon cancer and be completely asymptomatic and healthy.”
Early diagnosis, the second approach to the early detection of cancer, is much less resource intensive than screening as it targets individuals with symptoms to reduce delays in diagnosis and improve cancer outcomes. Although it is less effective than screening, early diagnosis can be used for many common cancers, including breast cancer, particularly in low-resource settings where screening may not be feasible.
To implement both screening and early diagnosis programs, population awareness, trained health care professionals, prompt referral systems, and appropriate diagnostic and therapeutic infrastructure are essential.
